Health impacts of the COVID-19 pandemic among Canadians living with
COVID 19 : impacts de la pandémie sur la santé des Canadiennes et Canadiens handicapé·es
Md Kamrul Islam,[1] PhD
The Prentice Institute for Global Population and Economy
University of Lethbridge, Alberta
md [dot] islam6 [at] uleth [dot] ca
Lars K. Hallstrom, PhD
Professor, Department of Political Science
Director, the Prentice Institute for Global Population and Economy
University of Lethbridge, Alberta
1lars [dot] hallstrom [at] uleth [dot] ca
Abstract
The devastating impact of the COVID-19 pandemic on general health has received extensive attention in recent research. However, limited attention has been given to examining the health impacts of the pandemic among people living with disabilities. This study examines the impact of the COVID-19 pandemic on three aspects of health among Canadians living with a disability: (1) perceived physical health, (2) perceived mental health, and (3) unmet healthcare needs during the pandemic. We utilized crowdsourcing data from Statistics Canada’s Impacts of COVID-19 on Canadians Living with Long-term Conditions and Disabilities, 2020 Survey. The total sample size for our study was 8,872 and included males and females who were 15 years and older. To examine the health impacts of the pandemic, we calibrated a multivariable logistic regression. We found that respondents living with a disability had higher odds of experiencing negative impacts from the pandemic on their physical and mental health and have more unmet healthcare needs than those without a disability. Youth (15–24 years) living with a disability had 4.11 times higher odds of experiencing poor physical health during the pandemic than older adults (65 years and older) without a disability. Similarly, respondents aged 25-44 years and 45-64 years living with a disability also had higher odds of experiencing poor physical health (5.34 times and 5.68 times respectively) during the pandemic than older adults without a disability. The health impacts of the pandemic among those living with disabilities were found to differ significantly by age cohorts.
Résumé
DL’impact dévastateur de la pandémie de COVID-19 sur la santé de la population générale a fait l’objet d’une grande attention dans les recherches récentes. Cependant, l’examen de l’impact de la pandémie sur la santé des personnes handicapées n’a fait l’objet que de peu d’attention. Cette étude examine l’impact de la pandémie de COVID-19 sur trois aspects de la santé des Canadiennes et Canadiens vivant avec un handicap : (1) la santé physique perçue, (2) la santé mentale perçue et (3) les besoins non satisfaits en matière de soins de santé pendant la pandémie. Nous avons utilisé des données d’un questionnaire en ligne provenant de l’étude de Statistique Canada intitulée « Répercussions de la COVID-19 sur les Canadiens vivant avec un problème de santé de longue durée ou une incapacité ». L’échantillon total de notre étude était de 8 872 personnes, hommes et femmes, âgés de 15 ans et plus. Pour examiner les effets de la pandémie sur la santé, nous avons calibré une régression logistique multivariable. Nous avons constaté que les personnes interrogées vivant avec un handicap étaient plus susceptibles de subir les effets négatifs de la pandémie sur leur santé physique et mentale, et d’avoir davantage de besoins non satisfaits en matière de soins de santé que les personnes sans handicap. Les jeunes (15 à 24 ans) vivant avec un handicap avaient 4,11 fois plus de chances d’avoir une mauvaise santé physique pendant la pandémie que les adultes plus âgés (65 ans et plus) sans handicap. De même, les répondant·es âgé·es de 25 à 44 ans et de 45 à 64 ans vivant avec un handicap avaient également plus de chances d’avoir une mauvaise santé physique (5,34 fois et 5,68 fois, respectivement) pendant la pandémie que les adultes plus âgés ne vivant pas avec un handicap. Nous avons constaté que les effets de la pandémie sur la santé des personnes vivant avec un handicap différaient considérablement selon les cohortes d’âges.
Keywords: Disability, physical health, mental health, unmet healthcare needs, COVID-19 pandemic
Introduction
The COVID-19 pandemic has created havoc in the lives and livelihoods of billions of people across the world. Although researchers have given extensive attention to the impact of the pandemic among general populations (Proto & Quintana-Domeque, 2021; Wang et al., 2021), few have examined those impacts on individuals living with a disability (Kavanagh et al., 2022; Schwartz et al., 2021). Within this modest literature, there is little discussion as to whether the health impacts of the pandemic among people with disabilities vary across different age cohorts. This study examines the impact of COVID-19 on three aspects of health for individuals living with a disability: physical health, mental health, and unmet healthcare needs during the pandemic. The research is guided by the following questions: (1) Are there significant differences in physical health among people during the pandemic by disability status? (2) To what extent has mental health during the pandemic varied by disability status? (3) Do peoples’ unmet healthcare needs during the pandemic vary significantly by disability status? (4) Do the impacts of the COVID-19 pandemic on physical health, mental health, and unmet healthcare needs, among people living with disabilities, vary significantly across different age cohorts? To address these questions, we utilized survey data from the Impacts of COVID-19 on Canadians Living with Long-term Conditions and Disabilities 2020, collected by Statistics Canada.
The COVID-19 pandemic has led to a wide range of negative impacts on the physical and mental health of general populations (Findlay, Arim, & Kohen, 2020; Shaukat, Ali, & Razzak, 2020), including decreased physical activity and well-being (Lesser & Nienhuis, 2020), and increased depression and anxiety (Porter et al., 2021), loneliness and social isolation (Hwang, Rabheru, Peisah, Reichman, & Ikeda, 2020), and stress associated with financial worries (Hertz-Palmor et al., 2021). People living with disabilities are more susceptible to the negative impacts of the pandemic on their health and are at greater risk of death (Kavanagh et al., 2022; Office for National Statistics, 2020). They may be more at risk of contracting COVID-19 and experiencing increased complications (Lebrasseur et al., 2021), and have reduced access to healthcare services (Kavanagh et al., 2022), decreased work opportunities (Emerson et al., 2021), and limited access to recreational and physical activities (Kamyuka, Carlin, McPherson, & Misener, 2020), when compared with the general population. Factors associated with disability such as higher prevalence of living alone, lower rates of internet use, and higher dependence on others for daily activities may compound the greater negative impacts of COVID-19 pandemic on health and well-being of persons living with disability (Statistics Canada, 2020a). In addition, discriminatory policies against people with disabilities may make them more vulnerable to the impacts of the pandemic (Adams, 2022).
Many people living with disabilities also have long-term chronic conditions (Gulley et al., 2018; Yokota et al., 2015) that may have further deteriorated due to inadequate access to required healthcare services during the pandemic. Health care services for those living with chronic conditions were interrupted during the pandemic due to reallocation of resources and decreased referral and hospitalization services (Danhieux et al., 2020; Kendzerska et al., 2021). Results from the 2020 COVID-19 Disability Survey in Canada showed that a majority of adult respondents with a disability (82%) experienced negative impacts on their mental health and experienced higher levels of social isolation (80%) compared with the general population. In addition, more than half of respondents became less physically active, and more than one-third described an increase in unhealthy lifestyle behaviour—smoking, drinking alcohol, and cannabis use (The Abilities Centre, 2020). Similarly, Pettinicchio, Maroto, Chai, and Lukk (2021) found that Canadians with disabilities and chronic conditions experienced increased anxiety (38.2%), stress (38.9%), and despair (18.1%) during the pandemic, and factors contributing to this decline in mental health included negative financial impacts, concerns about contracting COVID-19, increased loneliness, and a decreased sense of belonging.
The deleterious health impacts of the pandemic for people living with disabilities may have been further exacerbated due to higher unmet healthcare needs during the pandemic compared with the general population (Shakespeare, Ndagire, & Seketi, 2021). This gap has likely emerged due to limited access to healthcare services and medicine, postponement of some treatments and surgeries, inaccessible information and confusing guidance, financial constraints, and transportation barriers (Goggin & Ellis, 2020; Kibria, Islam, Miah, Ahmed, & Hossain, 2020; Uimonen et al., 2021). Results from the 2020 COVID-19 Disability Survey in Canada, conducted by the Abilities Centre (2020), showed that for more than half of the study participants, their needs for emotional counselling, specialized healthcare, case management, and attendant care were not met during the pandemic. Akobirshoev and colleagues (2022) revealed that adults with disabilities were at higher risk of experiencing disparities in delayed medical care and had higher unmet needs during the COVID-19 pandemic. Further research is needed to better comprehend the health impacts of the pandemic across different age cohorts living with disabilities.
The impact of the COVID-19 pandemic on the health of individuals may vary substantially across different age cohorts (Elder, Johnson, & Crosnoe, 2003; Elder, 1998; Settersten et al., 2020). For example, youth entering the labor force faced increased stressors during the pandemic due to reduced access to job opportunities (Lambovska, Sardinha, & Belas, 2021), and adults already in the labour market were living with uncertainties whether their jobs would continue, and challenges associated with maintaining families and societal responsibilities (Crayne, 2020). In contrast, older adults were at higher risk of complications and even death from the COVID-19 infection (Lee, 2020). While financial capacity clearly has implications for people’s health and well-being, older adults may have been advantaged compared with younger adults (Settersten et al., 2020). The differential impacts of the pandemic may be further exacerbated for people living with disabilities because the severity and cumulative effects of disabilities vary depending on the age at which they experienced the pandemic.
This study examines the health impacts of the COVID-19 pandemic across four age cohorts living with disabilities. We expected to find significant differences in the health impacts and unmet healthcare needs across the age cohorts living with a disability. Results from this study will provide important insights for developing strategies that tailor healthcare services to age-cohort specific needs of people living with disabilities.
Methods
Design
Data for this study came from Statistics Canada’s crowdsourcing survey on the Impacts of COVID-19 on Canadians Living with Long-term Conditions and Disabilities, 2020. The dataset provided information on income, expenses, general health, mental health, and unmet healthcare needs for 13,487 Canadians 15 years of age and older living with long-term conditions and disabilities, and it covered the ten provinces and territories.
Sample
For this study, we selected respondents living in five of the ten provinces: Nova Scotia, New Brunswick, Ontario, Alberta, and British Columbia. For our analysis, we excluded respondents from the remaining provinces because of coding differences in respondents’ age categories. The differences in age coding across provinces made it difficult to generate mutually exclusive age categories. We also excluded respondents living in the Territories because of very small number of cases; thus, the final sample size for this study was 8,872 respondents ages 15 years and older.
Dependent variables
There are five outcome variables of interest in this study: (1) perceived physical health during the pandemic, (2) perceived physical health compared with before the pandemic, (3) perceived mental health during the pandemic, (4) perceived mental health compared with before the pandemic, and (5) unmet healthcare needs during the pandemic.
The dataset contains information on physical and mental health since the start of the pandemic, which is reported into five categories: poor, fair, good, very good, and excellent. For this study, we coded the five categories into two: poor (comprising poor and fair) and good (comprising good through excellent) to represent people’s physical and mental health during the pandemic. The dataset also provides information on physical and mental health compared to before the pandemic into five categories: much worse now, somewhat worse now, about the same, somewhat better now, and much better now. These responses were coded into two categories: worse (comprising the first two categories) and not worse or same/better (comprising the last three categories) to represent people’s physical and mental health compared with before the pandemic. The outcome variables were coded as dichotomous to facilitate logistic regression analysis. The original distributions of the outcome variables were skewed to the left which violates the assumption of normal distribution for calibrating linear regression.
The dataset also provided information about whether respondents needed but did not receive healthcare services during the pandemic in the following areas: (1) physiotherapy/massage therapy/chiropractic, (2) speech therapy, (3) occupational therapy, (4) counselling from psychologist/social worker, (5) professional nursing care at home, (6) support groups/lines/addiction services, (7) medical testing unrelated to COVID-19, (8) medical treatments/appointments unrelated to COVID-19, (9) surgery, and (10) other therapies/services. Using this information, a dichotomous variable for unmet healthcare needs was created: yes (any of the 10 unmet needs) and no (none of the 10 unmet needs).
Independent variable
As part of Statistics Canada’s survey on the impacts of COVID-19 on Canadians, respondents were asked whether they identify as persons with a disability (yes or no). Using this information, the respondents’ disability status was coded into two categories: people with or without a disability. Disability is defined as the existence of a long-term or recurring impairment, such as vision, hearing, mobility, flexibility, dexterity, pain, learning, developmental, memory or mental health-related impairments that limit respondents’ daily activities (Statistics Canada, 2020b).
Covariates
Age cohorts were coded into four categories: 15–24 years, 25–44 years, 45–64 years, and 65 years and older. Information on respondents’ sex was reported under two categories: female and male. Among the control covariates, respondents’ level of education was reported into two categories: attended university vs. did not attend university. Respondents’ employment status before the pandemic was reported in three categories: employed, unemployed, and not in labour force. The information on employment status was recoded as dichotomous: employed vs not employed/not in labour force. We retained the original coding of monthly household income compared with before COVID-19: about same, increased, decreased, and not available.
Living arrangement was provided in three categories: (1) living alone, (2) multiple person household, no children, and (3) multiple person household, with children or all under 18 years old. The information on living arrangements was recoded into two categories: living alone vs. living with family/others (combining the second and third categories). The original coding of visible minority status was used for this analysis: visible minority vs. not a visible minority.
Information on community size was originally divided into six categories: 1,500,000+; 100,000 -499,000; 10,000 - 499,999; 500,000 - 1,499,99; Non-CMACA; 10,000 - 99,999 (any CMACA < 100,000). For our analysis, community size was coded as less than 1.5 million vs. 1.5 million or more. Finally, original coding of the provinces was used in the analysis: Nova Scotia, New Brunswick, Ontario, Alberta, and British Columbia.
The variables on living arrangement, employment status, and community size were coded as dichotomous to facilitate their inclusion in the regression analysis because of relatively small number of cases in some variables in the original categories.
Analysis
All of the outcome variables in this study were dichotomous. We carried out multivariable logistic regression analyses to examine the health impacts of the COVID-19 pandemic among Canadians living with disabilities. The logistic regression estimates were reported in the form of odds ratios (OR) with a 95% Confidence Intervals (CIs) and results that were statistically significant at the 0.05 level. We included an interaction term between disability status and age cohort to test whether the health impacts of the pandemic differed significantly by age cohorts. We have reported both the baseline model and the interaction model for the outcome variables in which the interaction effect was statistically significant. The total effects from interaction models—taking the main effects of disability status and age cohorts, and the interaction effect into account—were derived using Stata following the multiplicative approach for odds ratios (VanderWeele & Knol, 2014). In addition, adjusted predicted probabilities—derived based on setting each covariate to its mean values (Buis, 2007; Simon, 2013)—for the key independent variables (disability status and age cohorts) were also presented in graphs to better illuminate the health impacts of the pandemic among those living with disabilities.
The number of missing cases in the selected variables was very low (less than 3%) and a list-wise delete procedure was followed to deal with missing cases. In all analyses, the individual-level benchmarking factor (like the sampling weight) provided with the dataset was used to consider over/underrepresentation of the respondents by age, sex and province. However, because of the non-probabilistic nature of the crowdsourcing data, the results of this study cannot be applied to the overall Canadian population. Crowdsourcing is a new data initiative by Statistics Canada to generate timely information on important issues such as the impacts of COVID-19 on Canadians. In crowdsourcing, respondents visit Statistics Canada’s website and take part in online questionnaire surveys (Statistics Canada, 2020c). All analyses were carried out using Stata 17.0 data analysis software. Ethics approval was not needed for this study since it used only secondary sources of data.
Sample characteristics
More than half of the total respondents (59.6%) identified themselves as persons living with disability. The majority of the respondents were aged 45-64 years (36.3%) and female (69.5%). More than half of the respondents (50.8%) attended university and 52.4% were employed before the pandemic began. Over half of the respondents mentioned that their monthly household income had remained the same during the pandemic (59.2%) while 28.7% reported a decrease in their income, and 24.0% were living alone. Only 5.7% of the respondents identified as visible minorities, and more than three quarters of the respondents lived in communities of fewer than 1.5 million people. The majority of respondents lived in Ontario (70.2%), followed by British Columbia (13.9%) and Alberta (10.3%).
The sociodemographic distribution of the respondents by disability status showed that a slightly higher percentage of people living with disability were 45–64 years of age. Females had slightly higher percentage of living with disability. Those living with disability had lower percentages of attending university, engaging in employment, and being identified as visible minorities. In contrast, persons living with disability had higher percentages of reporting decreased income during the pandemic and living alone than those living without disability (Table 1).
| Characteristics | Sample Size (unweighted) | Total (N=8,872) | With Disability (N=5,315) | Without Disability (N=3,557) |
|---|---|---|---|---|
| Age cohorts (in years) | ||||
| 15-24 | 353 | 9.3 | 11.8 | 5.5 |
| 25-44 | 3,360 | 23.4 | 22.8 | 24.4 |
| 45-64 | 3,822 | 36.3 | 37.9 | 33.9 |
| 65+ | 1,337 | 31.1 | 27.5 | 36.2 |
| Sex | ||||
| Female | 7,454 | 69.5 | 70.8 | 67.5 |
| Male | 1,418 | 30.5 | 29.2 | 32.5 |
| Education | ||||
| Attended University | 4,693 | 50.8 | 44.2 | 60.6 |
| Did not attend University | 4,179 | 49.2 | 55.8 | 39.4 |
| Employment status before pandemic | ||||
| Employed | 5,496 | 52.4 | 44.8 | 63.7 |
| Not employed | 3,376 | 47.6 | 55.2 | 36.3 |
| Change in monthly household income compared with before COVID-19 | ||||
| About same | 5,028 | 59.2 | 58.0 | 60.9 |
| Increased | 620 | 6.6 | 7.4 | 5.4 |
| Decreased | 2,764 | 28.7 | 27.6 | 30.3 |
| Not available | 460 | 5.6 | 7.0 | 3.4 |
| Living arrangement | ||||
| Living alone | 2,021 | 24.0 | 26.4 | 20.6 |
| Living with family/others | 6,851 | 76.0 | 73.8 | 79.4 |
| Visible minority status | ||||
| Visible minority | 527 | 5.7 | 5.3 | 6.4 |
| Not a visible minority | 8,345 | 94.3 | 94.7 | 93.6 |
| Community size | ||||
| Less than 1.5 million | 6,809 | 77.4 | 78.1 | 76.5 |
| 1.5 million or more | 2,063 | 22.6 | 21.9 | 23.5 |
| Provinces | ||||
| Nova Scotia | 450 | 3.2 | 3.0 | 3.5 |
| New Brunswick | 243 | 2.4 | 2.5 | 2.2 |
| Ontario | 5,594 | 70.2 | 69.8 | 70.8 |
| Alberta | 936 | 10.3 | 10.7 | 9.9 |
| British Columbia | 1,649 | 13.9 | 14.1 | 13.7 |
| Total | 8,972 | 100.0 | 100.0 | 100.0 |
Note: 59.6% identified themselves as persons with disability
Results
Descriptive findings
Respondents living with a disability had larger percentages of experiencing poor physical health during the pandemic (59.2%) than those without disability (30.1%). Similarly, a greater percentage of respondents who lived with a disability experienced poor mental health during the pandemic (63.7%) than people living without a disability (49.2%). Respondents living with disabilities also had higher percentages of reporting worsening physical and mental health during the pandemic compared with before the pandemic. In addition, respondents living with disabilities were at higher risk of having unmet healthcare needs (83.1%) during the pandemic compared with people without disabilities (74.0%). Age-specific estimates showed that younger age cohorts experienced higher negative impacts of the pandemic on their physical and mental health compared to those aged 65 years and older (Table 2).
| |
|||||
| 15-24 | 25-44 | 45-64 | 65+ | Total | |
| Perceived poor physical health during the pandemic | |||||
|---|---|---|---|---|---|
| With disability | 57.9 | 60.7 | 63.2 | 53.0 | 59.2 |
| Without disability | 42.1 | 35.7 | 30.2 | 24.4 | 30.1 |
| Perceived worse physical health compared to before the pandemic | |||||
| With disability | 57.3 | 59.2 | 59.5 | 48.5 | 56.1 |
| Without disability | 51.3 | 47.3 | 42.2 | 32.3 | 43.9 |
| Perceived poor mental health during the pandemic | |||||
| With disability | 77.2 | 74.6 | 65.7 | 46.1 | 63.7 |
| Without disability | 78.5 | 66.4 | 51.3 | 31.5 | 49.2 |
| Perceived worse mental health compared to before the pandemic | |||||
| With disability | 71.9 | 71.9 | 64.9 | 47.1 | 62.4 |
| Without disability | 71.5 | 68.6 | 56.9 | 40.0 | 54.5 |
| Has unmet healthcare needs during the pandemic | |||||
| With disability | 77.7 | 86.3 | 84.5 | 80.9 | 83.1 |
| Without disability | 65.6 | 71.3 | 76.0 | 75.2 | 74.0 |
Multivariable findings
Perceived physical health during COVID-19 pandemic
Respondents living with a disability had 3.22 times higher odds of experiencing poor physical health during COVID-19 pandemic [95% CI: 2.52-4.12] than those without disability after adjusting for demographic, socioeconomic, and geographic characteristics. Younger age cohorts (15–24, 25–44, and 45–-64) had higher odds of experiencing poor physical health than adults 65 years and older (Interaction model on poor physical health in Table 3). Taking the significant interaction effects into account, along with the main effects of disability status and age, showed that respondents living with a disability and between 15–24 years of age had 4.11 times higher odds of experiencing poor physical health during the pandemic than adults 65 years and older without a disability. Similarly, respondents with a disability in the three other age cohorts (25–44, 45–64, and 65+ years) also had higher odds of experiencing poor physical health (5.34 times, 5.68 times, and 3.22 times respectively) during the pandemic than adults aged 65 years and older without a disability. The significant interaction term demonstrates that the combined effect of age and disability on poor physical health during the pandemic is greater than explained by the main effects alone.
| |
||||
| Baseline model on poor physical health | Interaction model on poor physical health | Baseline model on worse physical health | Interaction model on worse physical health | |
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| Disability status | ||||
|---|---|---|---|---|
| Yes | 2.90** [2.58-3.24] | 3.22** [2.52-4.12] | 1.70** [1.52-1.89] | 1.87** [1.48-3.35] |
| No | [REF] | [REF] | [REF] | [REF] |
| Age cohorts | ||||
| 15-24 years | 1.51** [1.14-2.00] | 2.44** [1.47-4.03] | 1.70** [1.29-2.23] | 2.34** [1.42-3.82] |
| 25-44 years | 1.87** [1.58-2.21] | 2.25** [1.75-2.89] | 1.87** [1.60-2.20] | 2.16** [1.72-2.72] |
| 45-64 years | 1.74** [1.49-2.03] | 1.68** 1.31-2.14] | 1.73** [1.49-2.01] | 1.74** [1.39-2.19] |
| 65+ years | [REF] | [REF] | [REF] | [REF] |
| Disability status* Age cohorts | ||||
| Yes* 15-24 years | 0.52* [0.29-0.93] | 0.64 [0.36-1.12] | ||
| Yes* 25-44 years | 0.74* [0.55-0.98] | 0.78 [0.59-1.03] | ||
| Yes* 45-64 years | 1.05 [0.78-1.41] | 0.98 [0.74-1.29] | ||
| No* 65+ years | [REF] | [REF] | ||
| Sex | ||||
| Female | 1.50** [1.30-1.73] | 1.49** [1.29-1.72] | 1.21** [1.05-1.38] | 1.20** [1.04-1.37] |
| Male | [REF] | [REF] | [REF] | [REF] |
| Education | ||||
| Did not attend university | 1.27** [1.14-1.42] | 1.28** [1.14-1.43] | 0.99 [0.89-1.11] | 0.99 [0.89-1.12] |
| Attended university | [REF] | [REF] | [REF] | [REF] |
| Employment status | ||||
| Not employed | 1.64** [1.44-1.87] | 1.65** [1.45-1.88] | 1.37** [1.21-1.56] | 1.38** [1.22-1.57] |
| Employed | [REF] | [REF] | [REF] | [REF] |
| Change in monthly HH income | ||||
| Increased | 1.54** [1.23-1.91] | 1.52** [1.22-1.89] | 1.86** [1.49-2.31] | 1.86** [1.49-2.30] |
| Decreased | 1.70** [1.49-1.92] | 1.71** [1.50-1.94] | 1.72** [1.52-1.94] | 1.73** [1.53-1.95] |
| Not available | 1.27 [0.98-1.63] | 1.28 [0.99-1.64] | 1.25 [0.97-1.59] | 1.25 [0.98-1.35] |
| About same | [REF] | [REF] | [REF] | [REF] |
| Living arrangement | ||||
| Living alone | 1.38** [1.21-1.56] | 1.37** [1.20-1.56] | 1.37** [1.21-1.56] | 1.37** [1.21-1.54] |
| Living with family/others | [REF] | [REF] | [REF] | [REF] |
| Visible minority status | ||||
| Visible minority | 1.15 [0.90-1.47] | 1.13 [0.88-1.43] | 0.92 [0.72-1.15] | 0.90 [0.72-1.16] |
| Not a visible minority | [REF] | [REF] | [REF] | [REF] |
| Community size | ||||
| 1.5 million or more | 0.97 [0.85-1.10] | 1.97 [0.85-1.11] | 1.18* [1.04-1.35] | 1.18* [1.03-1.35] |
| Less than 1.5 million | [REF] | [REF] | [REF] | [REF] |
| Provinces | ||||
| Nova Scotia | 0.89 [0.69-1.13] | 0.89 [0.69-1.13] | 0.92 [0.73-1.15] | 0.92 [0.72-1.16] |
| New Brunswick | 1.03 [0.74-1.45] | 1.03 [0.74-1.45] | 0.80 [0.59-1.09] | 0.80 [0.59-1.09] |
| Alberta | 1.05 [0.87-1.26] | 1.04 [0.87-1.25] | 0.99 [0.83-1.18] | 0.99 [0.83-1.18] |
| British Columbia | 1.21** [1.05-1.39] | 1.21** [1.05-1.40] | 0.98 [0.85-1.12] | 0.98 [0.85-1.12] |
| Ontario | [REF] | [REF] | [REF] | [REF] |
| Intercept | 0.13** [0.10-0.16] | 0.12** [0.09-0.15] | 0.27** (0.22-0.33) | 0.26** [0.20-0.32] |
| Adjusted Wald Test, F (df) | 39.23** (17, 8855) | 37.91** (20, 8852) | 19.16** (17, 8855) | 17.42** (20, 8852) |
| N | 8,872 | 8,872 | 8,872 | 8,872 |
* p < 0.05, ** p < 0.01
¥ The interaction effect of disability status and age cohorts on poor physical health was significant (p<0.002).
¥¥ The interaction effect of disability status and age cohorts on worse physical health was not significant (p=0.075).
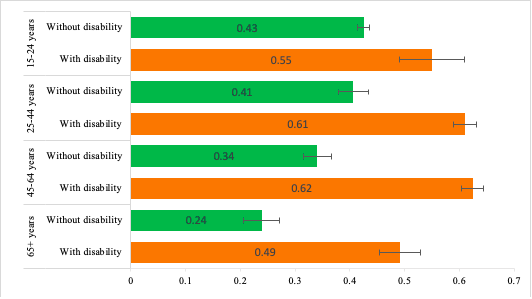
Figure 1 — derived based on the interaction model on poor physical health in Table 3 —shows that the adjusted predicted probability of experiencing poor physical health during the pandemic among respondents aged 15-24 years living with a disability was 0.55 which was 0.43 for those aged 15-24 years and without a disability. Respondents in other age cohorts with a disability also showed higher probability of experiencing poor physical health during the pandemic than those without a disability.
¥ The estimates are adjusted for respondents’ sex, education, employment status before the pandemic, change in monthly household income during the pandemic, living arrangements, visible minority status, community size, and province of residence.
Perceived physical health compared with before the COVID-19 pandemic
Respondents with a disability had 1.70 times higher odds of experiencing worse physical health when compared with before the pandemic [95% CI: 1.52-1.89] than those without a disability. Respondents in younger age cohorts had higher odds of experiencing worse physical health compared with before the pandemic than people aged 65 years and older. More specifically, those aged 15-24 years had 1.70 times higher odds of experiencing worse physical health [95% CI: 1.29-2.23] compared with before the pandemic than those aged 65 years and older. The odds of experiencing worse physical health compared with before the pandemic was even higher for those aged 25-44 years and 45-64 years (1.87 times and 1.73 times respectively) than those aged 65 years and older (baseline model on worse physical health in Table 3). In this case, only results from the baseline model on worse physical health were reported because the interaction effect of disability and age on worse physical health (compared with before the pandemic) was not significant, as shown in Table 3.
Perceived mental health during the pandemic
Respondents living with a disability had 1.70 times higher odds of experiencing poor mental health during the pandemic [95% CI: 1.35-2.14] than respondents living without a disability, even after adjusting for the covariates. Respondents in the younger age cohorts also had higher odds of reporting poor mental health since the start of the pandemic than those in the oldest age cohort (65+ years) (interaction model on poor mental health in Table 4). Taking the significant interaction effect into account with the main effects of disability status and age cohort showed that respondents with a disability, across all age cohorts, had higher odds of experiencing poor mental health than people 65 years of age and older without a disability. For instance, young adults (15–24 years) with a disability had 6.01 times higher odds of reporting poor mental health than adults 65 years and older who did not have a disability. Similarly, respondents in the three other age cohorts with a disability (25–44, 45–64, and 65+ years) also had higher odds of experiencing poor mental health (6.05 times, 3.96 times, and 1.69 times respectively) during the pandemic than adults aged 65 years and older without a disability. The significant interaction term demonstrates that the combined effect of age and disability on poor mental health during the pandemic is substantially different when explained by the main effects alone.
| |
||||
| Baseline model on poor mental health | Interaction model on poor mental healtha | Baseline model on worse mental health | Interaction model on worse mental healthb | |
| OR [95% CI] | OR [95% CI] | |||
| Disability status | ||||
|---|---|---|---|---|
| Yes | 1.53** [1.36-1.71] | 1.70** [1.35-2.14] | 1.24** [1.11-1.39] | 1.27* [1.01-1.58] |
| No | [REF] | [REF] | [REF] | [REF] |
| Age cohorts | ||||
| 15-24 years | 4.30** [3.16-5.86] | 7.01** [3.96-12.41] | 3.24** [2.44-4.30] | 3.81** [2.27-6.38] |
| 25-44 years | 3.98** [3.37-4.69] | 4.57** [3.61-5.78] | 3.17** [2.70-3.72] | 3.40** [2.71-4.28] |
| 45-64 years | 2.37** [2.03-2.75] | 2.41** [1.92-3.02] | 2.14** [1.85-2.48] | 2.07** [1.66-2.58] |
| 65+ years | [REF] | [REF] | [REF] | [REF] |
| Disability status* Age cohorts | ||||
| Yes* 15-24 years | 0.50* [0.26-0.97] | 0.80 [0.44-1.45] | ||
| Yes* 25-44 years | 0.78 [0.58-1.04] | 0.88 [0.67--1.16] | ||
| Yes* 45-64 years | 0.97 [0.73-1.28] | 1.06 [0.80-1.39] | ||
| No* 65+ years | [REF] | [REF] | ||
| Sex | ||||
| Female | 1.44** [1.25-1.65] | 1.43** [1.24-1.64] | 1.27** [1.10-1.45] | 1.26** [1.09-1.45] |
| Male | [REF] | [REF] | [REF] | [REF] |
| Education | ||||
| Did not attend university | 1.34** [1.19-1.50] | 1.34** [1.20-1.50] | 0.99 [0.89-1.11] | 0.99 [0.89-1.12] |
| Attended university | [REF] | [REF] | [REF] | [REF] |
| Employment status | ||||
| Not employed | 1.20** [1.05-1.37] | 1.21** [1.06-1.38] | 1.17* [1.03-1.33] | 1.17* [1.02-1.33] |
| Employed | [REF] | [REF] | [REF] | [REF] |
| Change in monthly HH income | ||||
| Increased | 1.66** [1.31-2.01] | 1.65** [1.30-2.09] | 1.39** [1.12-1.74] | 1.39** [1.11-1.73] |
| Decreased | 1.68** [1.47-1.90] | 1.69** [1.48-1.92] | 1.62** [1.43-1.84] | 1.63** [1.44-1.85] |
| Not available | 1.59** [1.20-2.09] | 1.60** [1.22-2.10] | 1.03 [0.80-1.33] | 1.03 [0.80-1.33] |
| About same | [REF] | [REF] | [REF] | [REF] |
| Living arrangement | ||||
| Living alone | 1.35** [1.18-1.54] | 1.34** [1.18-1.53] | 1.34** [1.18-1.52] | 1.33** [1.17-1.52] |
| Living with family/others | [REF] | [REF] | [REF] | [REF] |
| Visible minority status | ||||
| Visible minority | 1.22 [0.94-1.58] | 1.20 [0.93-1.56] | 0.92 [0.72-1.17] | 0.91 [0.71-1.16] |
| Not a visible minority | [REF] | [REF] | [REF] | [REF] |
| Community size | ||||
| 1.5 million or more | 1.09 [0.95-1.25] | 1.10 [0.95-1.25] | 1.13 [0.98-1.29] | 1.13 [0.98-1.29] |
| Less than 1.5 million | [REF] | [REF] | [REF] | [REF] |
| Provinces | ||||
| Nova Scotia | 0.85 [0.66-1.08] | 0.86 [0.67-1.09] | 0.85 [0.67-1.09] | 0.86 [0.67-1.09] |
| New Brunswick | 0.81 [0.58-1.13] | 0.81 [0.58-1.13] | 0.72* [0.53-0.99] | 0.72* [0.53-0.99] |
| Alberta | 1.02 [0.85-1.23] | 1.02 [0.85-1.22] | 1.07 [0.89-1.27] | 1.07 [0.89-1.27] |
| British Columbia | 1.00 [0.86-1.15] | 1.01 [0.86-1.16]] | 0.90 [0.78-1.04] | 0.90 [0.78-1.04] |
| Ontario | [REF] | [REF] | [REF] | [REF] |
| Intercept | 0.23** [0.19-0.29] | 0.22** [0.17-0.28] | 0.42** [0.35-0.52] | 0.42** [0.33-0.53] |
| Adjusted Wald Test, F (df) | 35.08** (17, 8855) | 30.89** (20, 8852) | 21.84** (17, 8855) | 18.99** (20, 8852) |
| N | 8,872 | 8,872 | 8,872 | 8,872 |
* p < 0.05, ** p < 0.01
a The interaction effect of disability status and age cohorts on poor mental health was significant (p<0.050).
b The interaction effects of disability status and age cohorts on worse mental health was not significant (p=0.371).
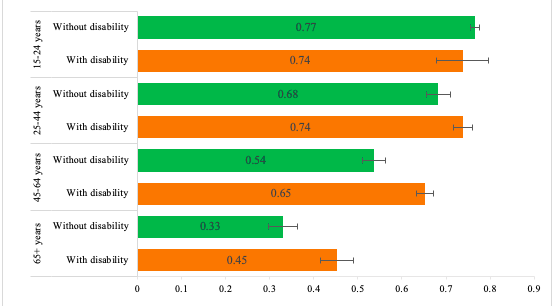
Figure 2—based on the interaction model on poor mental health in Table 4—shows that the oldest age cohort (65+ years) had the highest difference in the probability of experiencing poor mental health during the pandemic between those living with a disability and those living without a disability (0.45 and 0.33 respectively). In contrast, the youngest age cohort had the lowest difference in the probability of experiencing poor mental health during the pandemic between those living with a disability and those living without a disability (0.74 and 0.77 respectively).
¥ The estimates are adjusted for respondents’ sex, education, employment status before the pandemic, changed monthly household income during the pandemic, living arrangements, visible minority status, community size, and provincial residence.
Perceived mental health compared with before the pandemic
Respondents with a disability had 1.24 times higher odds of experiencing worse mental health when compared with before the pandemic [95% CI: 1.11-1.39] than respondents without a disability, after controlling for the other explanatory variables. Younger age cohorts had higher odds of experiencing worse mental health than the older age cohort of 65 years and older. The 15–24 age cohort, for example, had 3.24 times higher odds of reporting worse mental health [95% CI: 2.44-4.30] than the age cohort 65 years and older (model on worse mental health compared with before the pandemic in Table 4). Similarly, respondents aged 25-44 years and 45-64 years had higher odds of experiencing worse mental health (3.17 times and 2.14 times) compared with before the pandemic than those aged 65 years and older. Here, only findings from the baseline model on worse mental health were reported because the interaction effect of disability and age on worse mental health compared with before the pandemic was not significant, as shown in Table 4.
Unmet healthcare needs during the COVID-19 pandemic
Respondents living with a disability had 1.38 times higher odds of having unmet healthcare needs [95% CI: 1.04-1.82] than those living without a disability. The lower odds of having unmet healthcare needs during the pandemic among the youngest respondents (15–24 years) approached significance when compared with than older adults (65+ years) (interaction model of unmet healthcare needs in Table 5). Taking the significant interaction effect into account, along with the main effects of disability status and age, we noticed that respondents aged 25–44 years with a disability had 2.04 times higher odds of having unmet healthcare needs during the pandemic than respondents 65 years and older without a disability. Respondents in two other age cohorts (25–44 and 65+), with a disability, also had higher odds of having unmet healthcare needs during the pandemic (1.87 times and 1.38 times respectively) compared with people 65 years and older without a disability. The significant interaction term demonstrates that the combined effect of age and disability on unmet healthcare needs during the pandemic is greater than it would have been explained by the main effects alone.
| |
||
| OR [95% CI] | OR [95% CI] | |
| Disability status | ||
|---|---|---|
| Yes | 1.76** (1.53-2.03) | 1.38* [1.04-1.82] |
| No | [REF] | [REF] |
| Age cohorts | ||
| 15-24 years | 0.70* [0.51-.95] | 0.59 [0.35-1.00] |
| 25-44 years | 1.08 [0.89-1.31] | 0.80 [0.61-1.03] |
| 45-64 years | 1.21* [1.01-1.45] | 1.08 [0.83-1.39] |
| 65+ years | [REF] | [REF] |
| Disability status* Age cohorts | ||
| 1.36 [0.72-2.54] | ||
| Yes* 25-44 years | 1.85** [1.32-2.60]] | |
| Yes* 45-64 years | 1.25 [0.89-1.75] | |
| No* 65+ years | [REF] | |
| Sex | ||
| Female | 1.58** [1.35-1.85] | 1.60** [1.36-1.88] |
| Male | [REF] | [REF] |
| Education | ||
| Did not attend university | 0.83** [0.72-0.95] | 0.83** [0.71-0.94] |
| Attended university | [REF] | [REF] |
| Employment status | ||
| Not employed | 1.31** [1.12-1.55] | 1.29** [1.09-1.52] |
| Employed | [REF] | [REF] |
| Change in monthly HH income | ||
| Increased | 1.26 [0.96-1.64] | 1.26 [0.96-1.65] |
| Decreased | 1.82** [1.55-2.13]td> | 1.80** [1.53-2.11] |
| Not available | 1.03 [0.76-1.38] | 1.02 [0.75-1.37] |
| About same | [REF] | [REF] |
| Living arrangement | ||
| Living alone | 0.85* [0.72-0.99] | 0.86* [0.73-1.00] |
| Living with family/others | [REF] | [REF] |
| Visible minority status | ||
| Visible minority | 1.08 [0.82-1.44] | 1.09 [0.82-1.46] |
| Not a visible minority | [REF] | [REF] |
| Community size | ||
| 1.5 million or more | 1.09 [0.92-1.28] | 1.09 [0.93-1.28] |
| Less than 1.5 million | [REF] | [REF] |
| Provinces | ||
| Nova Scotia | 1.62** [1.17-2.23] | 1.62** [1.17-2.22] |
| New Brunswick | 1.29 [0.80-2.07] | 1.27 [0.79-2.03] |
| Alberta | 0.98 [0.78-1.23] | 0.98 [0.78-1.23] |
| British Columbia | 1.00 [0.83-1.20] | 0.99 [0.83-1.19] |
| Ontario | [REF] | [REF] |
| Intercept | 1.60** (1.26-2.01) | 1.81** (1.39-2.36) |
| Adjusted Wald Test, F (df) | 11.98** (17, 8855) | 13.02** (20, 8852) |
| N | 8,872 | 8,872 |
* p < 0.05, ** p < 0.01
¥¥ The interaction effect of disability status and age cohorts on unmet healthcare needs was significant (p<0.002).
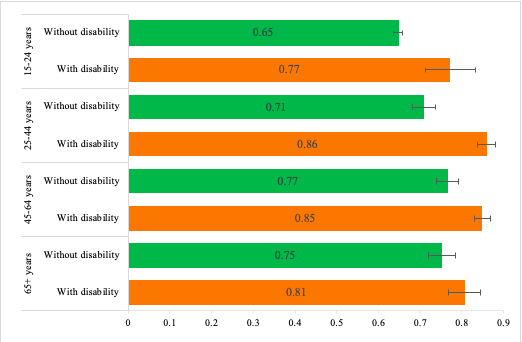
Figure 3—based on the interaction model in table 5—shows that the impacts of the pandemic on unmet healthcare needs among those living with a disability differ considerably across various age cohorts. For example, among the respondents living with a disability, those aged 25-44 years had the highest probability of having unmet healthcare needs (0.86) during the pandemic and those aged 15-24 years had the lowest (0.65). Respondents with a disability, across all age cohorts, had consistently higher probability of having unmet healthcare needs than their respective peers without a disability.
Note: The estimates are adjusted for respondents’ sex, education, employment status before the pandemic, changed monthly household income during the pandemic, living arrangements, visible minority status, community size, and provincial residence.
Results for other explanatory variables showed that females had higher odds of reporting poor physical health during the pandemic and worse physical health compared with before the pandemic than males. Similarly, respondents who were not employed, experienced decreases in income, or were living alone had higher odds of poor physical health during the pandemic and worse physical health compared with before the pandemic. This is also true in the case of those experiencing poor mental health during the pandemic and worse mental health compared with before the pandemic. The odds of having unmet healthcare needs were higher among females, those who were not employed, and for those who experienced decrease in their household income during the pandemic.
Discussion
This study examined the health impacts of COVID-19 pandemic across four age cohorts of people living with disabilities. We found substantial differences in the health impacts of the pandemic, between respondents living with a disability and those without a disability. Respondents living with a disability experienced greater negative impact from the pandemic on their physical health and mental health, and level of unmet healthcare needs. These findings are in accordance with existing research (Findlay et al., 2020; Shakespeare, Ndagire, & Seketi, 2021; Shaukat, Ali, & Razzak 2020; The Abilities Centre, 2020) and add further insight into the extent to which the impacts of the pandemic vary across various age cohorts on people living with a disability. Shakespeare and colleagues (2021) describe the vulnerabilities of people living with disabilities as “triple jeopardy”: higher risk of poor outcomes from exposure to COVID-19, limited access to regular healthcare, and adverse social impacts from pandemic mitigation measures. The authors identify several barriers that further exacerbated the vulnerabilities of people living with disabilities during the COVID-19 pandemic such as lack of adequate access to COVID-19 testing, sanitation, and hygiene facilities and postponement of essential medical treatment including rehabilitation.
One of the key findings of our study was the greater negative mental health impact of the COVID-19 pandemic on younger age cohorts (15–24 years and 25–44 years), with or without a disability, when compared with the oldest age cohort (65 years and older). Consistent with our findings, the OECD (2021) revealed that young people had 30% to 80% higher symptoms of depression or anxiety, in addition to higher levels of loneliness, than adults in Belgium, France, and the United States. There are several reasons for the greater negative impact of the pandemic on mental health among younger adults, including closure of educational institutions (Allemang, Cullen, Schraeder, Pintson, & Dimitropoulos, 2021), interruptions in daily routine and social interactions (OECD, 2021), loss of extracurricular activities (Courtney, Watson, Battaglia, Mulsant, & Szatmari, 2020; Lindsay & Ahmed, 2021), uncertainty about employment and missed career development opportunities (Lindsay & Ahmed, 2021), increased family violence (Usher, Bhullar, Durkin, Gyamfi, & Jackson, 2020), and limited access to mental health support (Mental Health Commission of Canada, 2020).
In connection with the higher negative health impacts of the pandemic, the Mental Health Commission of Canada (2020) revealed that 63.8% of youth (15–24) reported having poor mental health during the pandemic compared with 35% of adults 65 and older. To address the mental health issues facing youth, the Commission recommended adopting a multi-pronged approach that includes promoting youth engagement in schools, building capacity within schools to identify mental health challenges, encouraging parents to promote supportive home environments, strengthening community partnerships, and increasing funding to support social networks for youth. In addition, as suggested by Critical Disability Theory, instead of focusing on physical impairments of individuals attention should be given on addressing social norms that attach stigmatized attributes to individuals living with disability (Schalk, 2017).
The age-based disparities in the health impacts of COVID-19 pandemic may be also attributed to the greater career aspirations and sense of economic burden among youth (Arndt et al., 2006; Kornblith et al., 2007) and older adults’ experiences of dealing with adverse conditions and effective coping strategies (Brandtstadter, 1999; Na, Yang, Mezo, & Liu, 2022). Na and colleagues (2022) noticed that the youngest age cohort was the most vulnerable group for mental distress, with the highest perceived adversities and lowest resilience compared to older age cohorts. Studies that have looked at the impacts of COVID-19 pandemic among middle-aged adults (45-64 years) detected several factors that contributed to greater negative health impacts including fear and anxiety, household confinement, stress, and changing lifestyle (Chakrawarty et al., 2021; Wong et al., 2021; Kim & Crimmins, 2020).
However, this study has some limitations. Our study is based on crowdsourced cross-sectional survey data. Because of non-probabilistic sampling design of the crowdsourcing data findings of this study are represent only the study population. Using longitudinal data would have provided better insights into the health impacts of COVID-19 pandemic among people living with disabilities. Second, we did not carry out separate analyses for people living with physical, mental, and intellectual disabilities because of the smaller sample sizes in these sub-cohorts. Third, we did not look at the health impacts of the COVID-19 pandemic among racially marginalized people living with disabilities due to data limitations. Despite these caveats, our study does provide a comprehensive analysis and assessment of three aspects of health affected by the COVID-19 pandemic among people with disabilities: physical health, mental health, and unmet healthcare needs during the pandemic. Our examination of the interaction effect between disability status and age cohort better illuminates the extent to which health impacts of the pandemic vary across different age cohorts. The inclusion of multidimensional covariates in regression analyses illuminates the greater negative health impacts of the pandemic among females, those who are not employed or experienced decreases in household income.
Future research should focus on the health impacts of the COVID-19 pandemic among people living with disabilities by considering the number of disability related difficulties to depict the severity of the impact. Another important extension of this work should be examining the impacts of the pandemic among people living with disabilities based on number of unmet healthcare needs, to better illustrate their health-related vulnerabilities during the pandemic. Conducting qualitative studies on the health impacts of the pandemic among children living with disabilities would address another important lacuna in this field. Findings in this study may be useful for tailoring healthcare services to the needs of people living with disabilities and addressing their unmet healthcare needs.
Endnotes
References
- Adams, R. (2022). Urgent care: disability, pandemic, and the value of a life. The Lancet, 399(10323): 430-431. DOI: https://doi.org/10.1016/S0140-6736(22)00118-0.
- Akobirshoev, I., Vetter, M., Iezzoni, L. I., Rao, S. R., & Mitra, M. (2022). Delayed medical care and unmet care needs due to the covid-19 pandemic among adults with disabilities in the US. Health Affairs, 1;41(10):1505-12. DOI: https://doi.org/10.1377/hlthaff.2022.00509.
- Allemang, B., Cullen, O., Schraeder, K., Pintson, K., & Dimitropoulos, G. (2021). Recommendations for youth engagement in Canadian mental health research in the context of COVID-19. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 30(2), 123. PMID: 33953764; PMCID: PMC8056963.
- Arndt, V., Merx, H., Stegmaier, C., Ziegler, H., & Brenner, H. (2006). Restrictions in quality of life in colorectal cancer patients over three years after diagnosis: a population based study. European Journal of Cancer, 42(12), 1848-1857. DOI: https://doi.org/10.1016/j.ejca.2006.01.059.
- Brandtstadter, J. (1999). Sources of resilience in the aging self: toward integrating perspectives. In: Hess, T.M., Blanchard-Fields, F. (Eds.), Social Cognition and Aging. Elsevier, pp. 123–141. Carstensen, L.L., Shavit, Y.Z., Bar.
- Buis, M. L. (2007). Predict and adjust with logistic regression. The Stata Journal, 7(2): 221-226. https://journals.sagepub.com/doi/pdf/10.1177/1536867X0700700206.
- Chakrawarty, A., Ranjan, P., Klanidhi, K. B., Kaur, D., Sarkar, S., Sahu, A., ... & Wig, N. (2021). Psycho-social and behavioral impact of COVID-19 on middle-aged and elderly individuals: a qualitative study. Journal of Education and Health Promotion, 10. DOI: 10.4103/jehp.jehp_1458_20.
- Courtney, D., Watson, P., Battaglia, M., Mulsant, B. H., & Szatmari, P. (2020). COVID-19 impacts on child and youth anxiety and depression: Challenges and opportunities. The Canadian Journal of Psychiatry, 65(10), 688–691. DOI: https://doi.org/10.1177/0706743720935646.
- Crayne, M. P. (2020). The traumatic impact of job loss and job search in the aftermath of COVID-19. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S180. DOI: https://doi.org/10.1037/tra0000852.
- Danhieux, K., Buffel, V., Pairon, A., Benkheil, A., Remmen, R. et al. (2020). The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Family Practice. 2020;21:1–6. DOI: https://doi.org/10.1186/s12875-020-01326-3.
- Elder, G. H., Johnson, M. K., & Crosnoe, R. (2003). The emergence and development of life course theory. In J. T. Mortimer & M. J. Shanahan (Eds.) Handbook of the life course (pp. 3-19). Boston, MA: Springer. DOI: https://doi.org/10.1007/978-0-306-48247-2_1.
- Elder, G. H., Jr. (1998). The life course as developmental theory. Child Development, 69(1), 1–12. DOI: https://doi.org/10.2307/1132065.
- Emerson, E., Stancliffe, R., Hatton, C., Llewellyn, G., King, T., Totsika, V., . . . Kavanagh, A. (2021). The impact of disability on employment and financial security following the outbreak of the 2020 COVID-19 pandemic in the UK. Journal of Public Health,43(3): 472-478. DOI: https://doi.org/10.1093/pubmed/fdaa270.
- Findlay, L. C., Arim, R., & Kohen, D. (2020). Understanding the perceived mental health of Canadians during the COVTD-19 pandemic. Health Reports, 31(4), 22–27. DOI: https://www.doi.org/10.25318/82-003-x202000400003-eng.
- Goggin, G., & Ellis, K. (2020). Disability, communication, and life itself in the COVID-19 pandemic. Health Sociology Review, 29(2), 168–176. DOI: https://doi.org/10.1080/14461242.2020.1784020.
- Gulley, S. P., Rasch, E. K., Bethell, C. D., Carle, A. C., Druss, B. G., Houtrow, A. J., . . . Chan, L. (2018). At the intersection of chronic disease, disability and health services research: A scoping literature review. Disability and Health Journal, 11(2), 192–203. DOI: https://doi.org/10.1016/j.dhjo.2017.12.012.
- Hertz-Palmor, N., Moore, T. M., Gothelf, D., DiDomenico, G. E., Dekel, I., Greenberg, D. M., . . . Barzilay, R. (2021). Association among income loss, financial strain and depressive symptoms during COVID-19: Evidence from two longitudinal studies. Journal of Affective Disorders, 291, 1–8. DOI: https://doi.org/10.1016/j.jad.2021.04.054.
- Hwang, T.-J., Rabheru, K., Peisah, C., Reichman, W., & Ikeda, M. (2020). Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics, 32(10), 1217–1220. DOI: https://doi.org/10.1017/S1041610220000988.
- Kamyuka, D., Carlin, L., McPherson, G., & Misener, L. (2020). Access to Physical Activity and Sport and the Effects of Isolation and Cordon Sanitaire During COVID-19 for People With Disabilities in Scotland and Canada. Frontiers in Sports and Active Living, 2(183). DOI: https://doi.org/10.3389/fspor.2020.594501.
- Kavanagh, A., Hatton, C., Stancliffe, R. J., Aitken, Z., King, T., Hastings, R., . . . Emerson, E. (2022). Health and healthcare for people with disabilities in the UK during the COVID-19 pandemic. Disability and Health Journal, 15(1), 101171. DOI: https://doi.org/10.1016/j.dhjo.2021.101171.
- Kendzerska, T., Zhu, D. T., Gershon, A. S., Edwards, J. D., Peixoto, C. et al., (2021). The effects of the health system response to the COVID-19 pandemic on chronic disease management: a narrative review. Risk Management and Healthcare Policy, 14:575–84.
- DOI: https://doi.org/10.2147/RMHP.S293471.
- Kibria, G., Islam, T., Miah, S., Ahmed, S., & Hossain, A. (2020). Barriers to healthcare services for persons with disabilities in Bangladesh amid the COVID-19 pandemic. Public Health in Practice, 1, 100027. DOI: https://doi.org/10.1016/j.puhip.2020.100027.
- Kim, J. K., & Crimmins, E. M. (2020). How does age affect personal and social reactions to COVID-19: Results from the national Understanding America Study. PLoS One, 15(11), e0241950. DOI: https://doi.org/10.1371/journal.pone.0241950.
- Kornblith, A. B., Powell, M., Regan, M. M., Bennett, S., Krasner, C., Moy, B., ... & Winer, E. (2007). Long‐term psychosocial adjustment of older vs younger survivors of breast and endometrial cancer. Psycho‐Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer, 16(10), 895-903. DOI: https://doi.org/10.1002/pon.1146.
- Lambovska, M., Sardinha, B., & Belas, J., Jr. (2021). Impact of the COVID-19 pandemic on youth unemployment in the European Union. Ekonomicko-manazerske spektrum, 15(1), 55–63. DOI: dx.doi.org/10.26552/ems.2021.1.55-63.
- Lebrasseur, A., Fortin-Bédard, N., Lettre, J., Bussières, E.-L., Best, K., Boucher, N., . . . Routhier, F. (2021). Impact of COVID-19 on people with physical disabilities: A rapid review. Disability and Health Journal, 14(1), 101014. DOI: https://doi.org/10.1016/j.dhjo.2020.101014.
- Lee, Y. J. (2020). The impact of the COVID-19 pandemic on vulnerable older adults in the United States. Journal of Gerontological Social Work, 63(6-7), 559–564. DOI: https://doi.org/10.1080/01634372.2020.1777240.
- Lesser, I. A., & Nienhuis, C. P. (2020). The Impact of COVID-19 on Physical activity behavior and well-being of Canadians. International Journal of Environmental Research and Public Health, 17(11, 3899). DOI: https://doi.org/10.3390/ijerph17113899.
- Lindsay, S., & Ahmed, H. (2021). School and employment-related barriers for youth and young adults with and without a disability during the COVID-19 Pandemic in the Greater Toronto Area. Adolescents, 1(4), 442–460. DOI:https://doi.org/10.3390/adolescents1040034.
- Mental Health Commission of Canada. (2020). Lockdown life: Mental health impacts of COVID-19 on youth in Canada. Retrieved from https://www.mentalhealthcommission.ca/wp-content/uploads/drupal/2021-02/lockdown_life_eng.pdf.
- Na, L., Yang, L., Mezo, P. G., & Liu, R. (2022). Age disparities in mental health during the COVID19 pandemic: The roles of resilience and coping. Social Science & Medicine, 305, 115031. DOI: https://doi.org/10.1016/j.socscimed.2022.115031.
- OECD. (2021). Supporting young people’s mental health through the COVID-19 crisis. Electronic resource. Retrieved from https://read.oecd-ilibrary.org/view/?ref=1094_1094452-vvnq8dqm9u&title=Supporting-young-people-s-mental-health-through-the-COVID-19-crisis.
- Office for National Statistics. (2020). Updated estimates of coronavirus (COVID-19) related deaths by disability status, England: 24 January to 20 November 2020. Retrieved from https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbydisabilitystatusenglandandwales/24januaryto20november2020.
- Pettinicchio, D., Maroto, M., Chai, L., & Lukk, M. (2021). Findings from an online survey on the mental health effects of COVID-19 on Canadians with disabilities and chronic health conditions. Disability and Health Journal, 14, 101085. DOI: https://doi.org/10.1016/j.dhjo.2021.101085.
- Porter, C., Favara, M., Hittmeyer, A., Scott, D., Sánchez Jiménez, A., Ellanki, R., . . . Stein, A. (2021). Impact of the COVID-19 pandemic on anxiety and depression symptoms of young people in the global south: evidence from a four-country cohort study. BMJ Open, 11(4), e049653. DOI: http://dx.doi.org/10.1136/bmjopen-2021-049653.
- Proto, E., & Quintana-Domeque, C. (2021). COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLoS One, 16(1), e0244419. DOI: https://doi.org/10.1371/journal.pone.0244419.
- Schalk, S. (2017). Critical Disability Studies as Methodology. Lateral, 6(1). DOI: https://doi.org/10.25158/L6.1.13.
- Schwartz, A. E., Munsell, E. G., Schmidt, E. K., Colón-Semenza, C., Carolan, K., & Gassner, D. L. (2021). Impact of COVID-19 on services for people with disabilities and chronic health conditions. Disability and Health Journal, 14(3), 101090. DOI: https://doi.org/10.1016/j.dhjo.2021.101090.
- Settersten, R. A., Jr., Bernardi, L., Härkönen, J., Antonucci, T. C., Dykstra, P. A., Heckhausen, J., . . . Thomson, E. (2020). Understanding the effects of Covid-19 through a life course lens. Current Perspectives on Aging and the Life Cycle, 45, 100360-100360. DOI: https://doi.org/10.1016/j.alcr.2020.100360.
- Shakespeare, T., Ndagire, F., & Seketi, Q. E. (2021b). Triple jeopardy: disabled people and the COVID-19 pandemic. The Lancet, 397(10282), 1331-1333. DOI: https://doi.org/10.1016/S0140-6736(21)00625-5.
- Shaukat, N., Ali, D. M., & Razzak, J. (2020). Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. International Journal of Emergency Medicine, 13(1), 40. DOI: https://doi.org/10.1186/s12245-020-00299-5.
- Simon, S. (2013). Calculating predicted probabilities from a logistic regression model. http://www.pmean.com/13/predicted.html.
- Statistics Canada. (2020a). Vulnerabilities of Canadians with disabilities during the COVID-19 pandemic. The Daily, July 6. https://www150.statcan.gc.ca/n1/en/daily-quotidien/200706/dq200706a-eng.pdf?st=55hslyj3.
- Statistics Canada. (2020b). Crowdsourcing: Impacts of COVID-19 on Canadians Living with Long-term Conditions and Disabilities. https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5323.
- Statistics Canada. (2020c). Impacts of COVID-19 on Canadians: First results from crowdsourcing. The Daily, April 23. https://www150.statcan.gc.ca/n1/en/daily-quotidien/200423/dq200423a-eng.pdf?st=Mgaj1Lp0.
- The Abilities Centre. (2020). COVID-19 Disability Survey. Retrieved from https://abilitiescentre.org/Abilities/media/Documents/Covid-survey-report-Dec-18_1.pdf.
- Uimonen, M., Kuitunen, I., Paloneva, J., Launonen, A. P., Ponkilainen, V., & Mattila, V. M. (2021). The impact of the COVID-19 pandemic on waiting times for elective surgery patients: A multicenter study. PLoS One, 16(7), e0253875. DOI: https://doi.org/10.1371/journal.pone.0253875.
- Usher, K., Bhullar, N., Durkin, J., Gyamfi, N., & Jackson, D. (2020). Family violence and COVID-19: Increased vulnerability and reduced options for support. International Journal of Mental Health Nursing, 29(4), 549-552. DOI: https://doi.org/10.1111/inm.12735.
- VanderWeele, T. J., & Knol, M. J. (2014). A tutorial on interaction. Epidemiologic Methods, 3(1), 33-72. DOI: https://doi.org/10.1515/em-2013-0005.
- Wang, C., Tee, M., Roy, A. E., Fardin, M. A., Srichokchatchawan, W., Habib, H. A., . . . Le, X. T. (2021). The impact of COVID-19 pandemic on physical and mental health of Asians: A study of seven middle-income countries in Asia. PLoS One, 16(2), e0246824. DOI: https://doi.org/10.1371/journal.pone.0246824.
- Wong, Z. X., Phua, A., Chew, K. A., Mohamed, J. S., Pérez, K. M., Mangialasche, F., ... & Chen, C. (2021). Impact of Covid‐19 pandemic on lifestyle in a middle‐aged and elderly population. Alzheimer's & Dementia, 17, e057643. DOI: https://doi.org/10.1002/alz.057643.
- Yokota, R. T. C., Berger, N., Nusselder, W. J., Robine, J.-M., Tafforeau, J., Deboosere, P., & Van Oyen, H. (2015). Contribution of chronic diseases to the disability burden in a population 15 years and older, Belgium, 1997–2008. BMC Public Health, 15(1), 229. DOI: https://doi.org/10.1186/s12889-015-1574-z.