Diabetes, Art, and Data Resonance
Diabète, art et résonance des données
Samuel Thulin
Independent Artist and Researcher
samuel_thulin [at] yahoo [dot] ca
Abstract
This paper presents the project Hemo-resonance #1, the first in a series of art works that aim to open alternative pathways for thinking about and practicing diabetes. I begin by discussing the centrality of data collection via self-tracking for the management of Type 1 diabetes, and the ways this data collection orients understandings of diabetes and the diabetic body. Diabetic self-management is typically aimed at finding patterns in one’s data, establishing cause and effect relationships, and understanding trends in the body’s operation so that the diabetic can modulate behaviour to optimize health outcomes. Arguing that approaching data in different ways can provide insights into diabetic experience and relationships that extend beyond the goal-oriented approach of always doing better, I offer “data resonance” as a way of following other trajectories of data and bodies. Data resonance provides sensory-rich materialisations of data in ways that seek to detach themselves from the typical focus on the legibility or interpretability of the data. This suspension of habitual orientations to data makes space for thinking of bodies, data, and the relationships between the two in new ways, and offering meditations on the value of co-corporeality, human-non-human relationships, and bodily difference.
Résume
Cet article présente le projet Hémo-resonance no 1, le premier d’une série d’œuvres d’art qui visent à ouvrir des voies alternatives pour penser et pratiquer le diabète. Je commence par discuter de la centralité de la collecte de données via l’auto-suivi pour la prise en charge du diabète de type 1, et de la manière dont cette collecte de données oriente la compréhension du diabète et du corps diabétique. L’autogestion du diabète vise généralement à trouver des tendances dans ses données, à établir des relations de cause à effet et à comprendre les schémas de fonctionnement du corps afin que la personne diabétique puisse moduler son comportement dans le but d’optimiser les résultats pour sa santé. Arguant qu’en approchant les données d’autres façons on peut fournir de l’information sur l’expérience et les relations diabétiques qui s’étendent au-delà de l’approche axée sur les objectifs consistant à toujours s’améliorer, je propose la « résonance des données » comme moyen de suivre d’autres trajectoires de données et de corps. La résonance des données fournit une matérialisation riche en sensorialité des données de manière à se détacher de l’accent typiquement mis sur leur lisibilité ou leur interprétabilité. Cette suspension des orientations habituelles pour les données fait de la place à une nouvelle façon de penser les corps et les données ainsi que les relations entre les deux, et propose de réfléchir à la valeur de la co-corporalité, des relations entre humain et non-humain et de la différence corporelle.
Keywords: diabetes, self-tracking, data, art, invisible disability, chronic illness, vibration, resonance
Introduction
This paper presents the project Hemo-resonance #1, the first in a series of art works that aim to open alternative pathways for thinking about and practicing diabetes.[1] As a chronic illness requiring regular healthcare appointments and continuous self-management, Type 1 diabetes is not easy to situate outside the frame of medicine. To explain Type 1 diabetes is to rely on medical language – it is a condition in which the beta cells of the pancreas no longer produce adequate amounts of insulin. Since the body requires insulin to process carbohydrates for energy, without it the body’s metabolism is seriously disrupted, potentially leading to death if insulin is not administered regularly via injections or insulin pump therapy. Given the severe consequences of lack of medical treatment, it is not surprising that a biomedical perspective is predominant in orienting understandings of diabetes. This is a perspective that privileges ideals of control and the potential of emergent technologies to improve diabetic outcomes, offering people with diabetes the promise of a more “normal” life. Without arguing against the necessity of diabetic treatment, I contend that it is nonetheless necessary to explore other ways of understanding diabetes – ways that consider what diabetes has to offer as a mode of being in the world, and that are attuned to the “generative possibilities for world-making among those living with diabetes” (Bennet, 2019, p. 25). Hemo-resonance #1 is an attempt to make space for considering diabetes in ways not driven primarily by achieving tighter control and improved outcomes. It is a creative modulation of my diabetic practice that attempts to suspend orientation towards particular end-goals and dwell in some of the lesser-explored resonances of diabetes.
Hemo-resonance #1 is situated at the intersection of art, chronic illness, disability, and the increasing prevalence of body-related data produced through self-tracking. The work bears some affinities to Shimon Attie’s White Nights, Sugar Dreams (2000), a notable example of media art taking up Type 1 diabetes. Attie’s work combines phantasmagorical images and the narratives of multiple people with Type 1 diabetes, creating an intersubjective meditation on chronic illness that is irreducible to a medical model. Of the work, Kuppers (2007) notes, “This is not a new paradigm of what diabetes is, offering itself as an alternative to the monolithic ideas of pathology and tragedy. Instead, multiplicity undermines or at least destabilizes any one capturing image” (p.50). Like Attie, I want to propose myriad trajectories for diabetic experience and practice, and in doing so I feel it appropriate to move between critique of the single-mindedness of much diabetic treatment, and the creation of possibilities that exist on their own terms on a terrain where there is no need for normative argumentation.
While Attie’s poly-voiced work lends itself especially well to multiplicity by bringing together different people’s stories, I have been concerned with finding multiplicity even within one person’s diabetic practice and experience. This is motivated by the relationship between diabetic self-monitoring and the larger social and cultural emphasis on self-tracking for the primary goal of improving one’s health and fitness, visible through the rapid uptake of apps and devices such as MyFitnessPal and Fitbit (Elman, 2018; Lupton, 2014b; Maturo et al., 2016;). Diabetic self-management, including self-tracking, is viewed as “the cornerstone of care” for diabetes (Clark, 2008), and a valuable area for investigating the notions of patient empowerment and entrepreneurship (sometimes referred to as Patient 2.0) that are often attributed to new monitoring technologies and practices (Bruni & Rizzi, 2013; Moretti & Morsello, 2017). In this context, my choice to work with my own diabetic data puts Hemo-resonance #1 in dialogue with the goals of individual achievement omnipresent in self-tracking discourses and practices, and with the ideals of self-empowerment associated with Health 2.0. That said, I am wary of the ways the improved outcomes championed by self-management agendas using the latest technologies are built on an orientation to the body that sees it, in one way or another, as something that should be always made “better” than what it currently is. The intense focus on tracking physical performance – whether running a marathon or keeping one’s blood sugar levels in check (or doing both at the same time) – fosters ableist orientations to bodily data that have the effect of marginalizing and devaluing bodily difference. The space I aim to create through Hemo-resonance #1 is one that while remaining in touch with diabetic treatment and the larger cultural imperatives of health and fitness, offers other ways of approaching data and bodies, following resonances between them for purposes apart from predestined self-improvement.
While perspectives on the “diabetes data revolution” (Kowalski, 2019) typically focus on more – and more accurate – data for purposes of improved decision-making and device automation, leading to better blood-sugar control, Hemo-resonance #1 is more concerned with how “the production of data about our bodies is an inventional, on-going process” (Gouge & Jones, 2018, p. 427). In other words, rather than focussing on end goals for data collection, it explores the creative potential of diabetes as a set of practices that shed new light on how bodies and data modulate each other. I have found that making artwork with the data that I normally use to guide my day-to-day life as diabetic inflects my relationship to diabetes, to my body, and to data. This offers possibilities that are not in opposition to treatment but that are in opposition to the idea that diabetes needs to be unilaterally oriented by the quest to match the standards of a “normal” body.
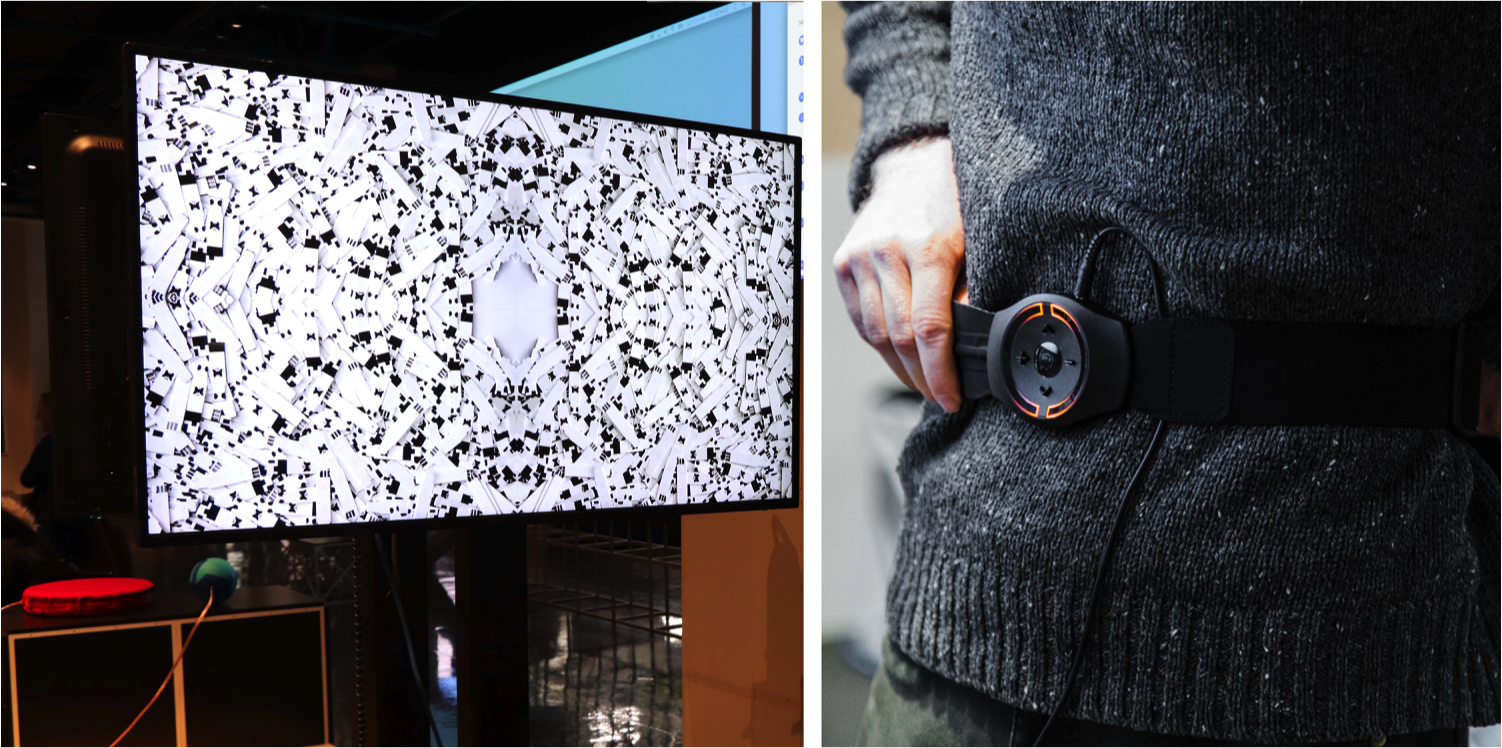
Hemo-resonance #1 presents my blood glucose readings and insulin injection amounts from a period of 100 days as resonant data. The numbers (mmol/l blood glucose concentration and units of insulin injected) are converted to vibrations that can be simultaneously felt by viewers via vibrotactile objects and seen in a video of a kinetic visualization process. The visualization shows the effects of the vibrafied data as they are channeled to a resonant surface on which the used blood sugar test-strips from the 100 day period are spread out. The hundreds of black and white (and occasionally blood stained) test strips – each about 0.5 cm wide and 3 cm long - tremble and move across the screen in kaleidoscopic patterns. Meanwhile, the visitor feels vibrations emanating from two devices as they hold them against their body– I have experimented both with DIY vibrotactile cushions and with a commercial haptic system called Woojer. Long, low-frequency vibrations are felt from one device in response to the amount of insulin in my body throughout the 100 day period. More punctual, percussive, higher-frequency vibrations are felt from the other device in response to my blood-sugar level fluctuations over the same time period. The movements and sensations of bodily data prompt questions about how we create and orient ourselves by data, and what this means for how we live and understand bodily difference.
Living With Numbers
Bodily and health-related data are increasingly part of life for both diabetics and non-diabetics. The data generated by various self-tracking activities are used to simultaneously provide a window into the functioning of one’s body and motivation for the improvement of that functioning. This is perhaps nowhere more evident than in the Quantified Self movement, with its motto “Self knowledge through numbers”. Quantified Selfers are at the forefront of self-tracking, coming up with an ever-increasing array of things to track and ways of interpreting the data. This purportedly improved self-knowledge allows individuals to act on their bodies in the hopes of improving their lives. As Smith and Vonthehoff (2017) note, self-tracking is deeply linked to a way of conceptualizing the body that “positions it as an ongoing project that demands the investment of attentiveness and labour, and the consumption of enrichment goods and services” (p.13). Not surprisingly, the movement includes some diabetic members, as well as non-diabetics who have chosen to track their blood sugar. Founder and non-diabetic Gary Wolf tracks his blood-glucose and has used the data to determine that he might be pre-diabetic. Here, numbers are taken to offer an enlightened perspective on the body that is otherwise an unreliable narrator and/or harbouring deep secrets. As Lupton (2013) puts it, “The self-knowledge that is viewed as emerging from the minutiae of data recording a myriad of aspects of the body is a psychological salve to the fear of bodily degeneration” (p.397). Lupton (2013; 2017) and Smith and Vonthehoff (2017) assert that self-tracking is linked to a distrust of the sensation of the body and the attempt to get at a less capricious source of knowledge.
Diabetic self-tracking emerged prior to the Quantified Self movement and there is no necessary affiliation between people with diabetes and the Quantified Self community. Following Lupton’s taxonomy of self-tracking, diabetics often correspond most closely with the notion of “pushed self tracking”, where external encouragement, in this case from a healthcare provider, is a major determining factor in the self-tracking activities (Lupton 2014a; Piras & Miele, 2017). As with non-diabetic self-tracking, the goal remains acquiring knowledge of the body through numbers in order to forestall bodily decline. But the centrality of self-tracking to diabetes management makes the import of numbers particularly acute. Numbers, especially blood-glucose levels determined either from a glucometer or continuous glucose monitor, are used both as indicators of success and as mediators of control, revealing how well one has been managing their diabetes and informing future action for achieving target results. The consequences of uncontrolled diabetes range from complications due to frequent high blood sugar, such as nerve damage and kidney failure, to the immediate dangers of low blood sugar, including loss of consciousness and death.
The predominant biomedical perspective approaches numbers both as objective and as necessary for bodily intervention. This intervention is expansive. The diabetic becomes aware of her body in new ways through diabetic self-management achieved via the collection of diagnostic data and a repertoire of intentional responses to the available data. What was once an unconscious, internal, metabolic process (processing sugar to produce energy), becomes a conscious practice that extends beyond the boundary of the skin, and that proliferates data, (finger-pricks, injections), and increasingly networked decision-making. Performing a reconfigured and numerically-dependent body, the diabetic, in collaboration with an array of humans (health care providers, family members, friends) and devices (glucose meters, syringes, pens, insulin pumps, continuous glucose monitors), takes responsibility for achieving what was once the purview of one of his organs. He is invited to “Think like a pancreas” (Scheiner, 2011), acting to restore the normal functioning associated with the now-ineffective body part.
The numbers involved in self-management are highly embodied in multiple ways, bridging physical sensation and emotional responses. Despite the notion of a split between bodily sensation as subjective and numbers as objective that characterizes many discussions of self-tracking, Lupton (2017) has described the ways in which numbers nonetheless intertwine with bodily feelings, as part of what she refers to as “data sense”. As she puts it, “Data sense, therefore involves entanglements of human senses and digital sensors with sense-making. This approach underlines the embodied, affective, and material nature of engaging with and learning from data (Fors et al., 2013; Sumartojo et al., 2016)” (Lupton, 2017, p. 1604). In my own diabetes self-management, numbers have complex physical and emotional registers developed through years of hourly engagement with them. For instance, numbers like 3.4 or 2.7 are associated with the weakness, irritability, desperation, hunger, and inability to think that I feel when I have low blood glucose. But such numbers can also bring feelings of relief, as they offer an explanation for why I feel so bad, as well as frustration and disappointment for falling below my target range. These numbers and feelings travel beyond my body, too, as those who know me well can often tell that I am low before I become aware of it myself; they might suggest I check, and having done so I will affirm, “you’re right, I am 3.1”.
As Arduser (2017) puts it: “Once the technology of home meters and blood glucose test strips became available, people with diabetes not only learned to rely on numbers to determine their level of control as they performed the time-consuming tasks of self-managing their disease but they also learned to communicate about their disease through numbers” (p.35). Arduser goes on to note how this heavy reliance on numbers relates to identity and morality, as a marker of how well the diabetic is doing. Bad numbers can become internalized as bad behaviour, with the diabetic casting themselves (and being cast by medical discourse) in the role of bad patient (p. 37). The blood sugar test thus operates not only to check blood-glucose levels. Through the resultant number, the test also acts as an assessment of one’s knowledge in treating their diabetes and their level of morality and responsibility in attaining the appropriate knowledge and putting it to good use. As Bennett (2019) shows, attaining exceptionally good blood-sugar levels can make one a “super crip” (p. 40), where diabetic management is a performance that proves one’s personal capacities through numbers. With all these layers of numerical significance, uncoupling embodied feelings – physical and emotional– from numbers is next to impossible, despite the fact that the powerful and complex resonances of numbers are rarely investigated in depth in clinical settings, where diagnostic utility is more highly valued.
A Diabetic Body by Numbers
As tools for visualizing the interior spaces of the body and for modulating bodily awareness and sensation, numbers are supremely personal. Smith (2016) has referred to the data that comes from our bodies as a type of “disembodied exhaust” that we cannot help but produce in the current datafied context. But the more germane aspect of his theorization for my purposes is his discussion of the leakiness of bodies that takes place through the emitting of this data (p. 111). Here, numbers may be thought of as a kind of liquid that trespasses the skin barrier of bodies, recalling aspects of the body that provoke a kind of unease or disgust (see Lupton’s (2012) discussion of “Cleanliness, Dirt and Symbolic Body Boundaries” (pp. 34-37)). There’s an excessive intimacy in bodily data as it spills over established boundaries of bodies. Its common figuration as numbers, graphs, charts, etc., tames it, rendering it something objective, excised from the body, made clean, controllable, and most importantly useful for the further controlling of bodies – for making decisions about bodies, based on this trickling data. As van der Ploeg (2012) contends, new bodies are emerging. These are bodies so intertwined with information that it may be difficult to tell where the body ends and data begins, and vice versa. Horrocks (2019) notes that the increasing swaths of numerical data used in diabetic management contribute to producing Datafied Body Doubles as attempts to recreate the dynamic physiologies of Type 1 diabetes in data form.
Diabetic data diverges from much tracked body-related data in that the processes involved in its collection breach the body in particularly intimate ways. It is not a sensor resting on the skin, or a distant surveillance apparatus that allows for the crucial insights on the body. Instead, material from the body– blood – needs to be extracted before data can be extracted from that material. Or, in the case of continuous glucose monitors, the device penetrates the skin in a more sustained fashion, bridging external worlds and internal body processes. Similarly, while it is common for self-trackers to record what they put in their bodies through the traditional route of consumption (what they eat), diabetics also record the liquids they inject that breach the skin (insulin). Diabetic data is oriented by the metabolic body in process. As Mol and Law (2004) note, the metabolic body incorporates and excorporates its surroundings, such that body boundaries are troubled. Taking on the work of the pancreas means that the processes the pancreas regulates weave in and out of the skin, drawing the body into relations with other technologies and interactions. It involves diabetic “data rituals”, the term Laura Forlano (2017) uses to describe the combination of data practice, phenomenological lived experiences, and labour involved in diabetic self-management. Diabetic data tracks the diabetic body’s “abnormal” and multiple entanglements with the world, its extended fluid exchange through piercing the skin and communicating via numbers. Many forms of self-tracking risk taking the fleshy body as a given to be observed, and/or they assume boundaries that will not be crossed (in monitoring one’s heart rate for example, the heart is an object residing within the body whose activity can be quantified). Diabetic data tracking reminds us in concrete terms of the fluidity of the body – that as Mol and Law (2004) say, a lot of work is involved in simply holding a body together (p. 57).
It is in the acts of blood sugar testing and insulin injection that the diabetic body also moves from invisibly disabled to visibly disabled and back again several times a day. This habitual disclosure is modulated depending both on practical circumstances and on each diabetic’s relation to self and others. Mol (2009) talks of a construction worker who simply does not have the time/space/conditions to test his blood-sugar as often his health care practitioner asks him to (p. 1757). On online forums, there are perennial discussions around how people approach testing and injecting in public, and discussions of the reactions of non-diabetics. These are questions of how to negotiate the extended body (which is also viewed as a vulnerable body by many, despite counter-discourses on how diabetes has made them stronger), the body whose practice has become excessive in the context of commonly held attitudes positing that blood should stay within the body, and things should not enter by way other than the mouth.
Wearable and networked technologies (such as insulin pumps, continuous glucose monitors, and apps) increasingly offer new possibilities for people with diabetes to avoid the awkwardness of managing their illness in public, as direct bodily intervention can be replaced by innocuous interactions with smart phone apps. Such developments point to the complexity of diabetes’ relationship to disability and the way it is modulated by data practices. Many diabetics do not identify as disabled (Forlano, 2017, p. 4; Kafer, 2013, p. 14), and certainly identification is complicated both by the potential for diabetics to “pass” (Samuels, 2003) as non-disabled much of the time, and by the complex relationship between disability and chronic illness (Wendell, 2001). The current data-mediated management of Type 1 diabetes simultaneously fosters avenues for its increased invisibility and doubles-down on the position that the body can and should be made as “normal” as possible through technological intervention. Here, whether diabetes is considered a disability or not, approaching it from a critical perspective aligns with critical disability studies in recognizing how ableist attitudes towards health and the body evacuate the possibilities for seeing value in human variation. Rather than understanding diabetes as a valuable way of being the world, the push to get it under control and out of sight – however well-intentioned – is steeped in representations of illness and disability that see them as threats to normalcy and idealized notions of selfhood.
Tracking the representation of disability and its conflict with American ideology, Garland-Thomson notes “ Seen as a victim of alien forces, the disabled figure appears not as transformed, supple, or unique, but as violated. In contrast, the autonomous individual is imagined as having inviolate boundaries that enable unfettered self-determination creating a myth of wholeness” (p. 45). Autonomy and self-containment are challenged by the diabetic body and its circulation of fluids and data. The self-management practices involved in daily life with diabetes demonstrate the relationality of the self and its extension beyond the skin boundary rather than presenting a complete, easily identifiable and delineated, autonomous self in total control of its being. At the same time, if as Garland-Thomson argues, “the disabled body stands for self gone out of control” (p. 43), ironically the work the diabetic engages in to control the body becomes the very signal of the body’s otherness and disability. It is the process of reigning in the body that reveals how it has become excessively interwoven with things that appear traditionally ‘outside itself’, and how it spills itself into the world. The more the diabetic tries to maintain control the more she signals to the world a body that has lost control and must be supplemented by various measures – refusing to eat when offered, eating at socially inappropriate times, testing blood sugar levels, injecting insulin, etc. Yet, outside of these breaching performances of self-management the diabetic passes as “normal”, whether she would choose to or not.
Until now, I have been describing a largely anonymous diabetic body. However , no such generalized body exists. There are only actual diabetic bodies, and many of them. Emphasizing the importance of physically situated knowledge, Arduser (2017) argues “understanding the disease is important, but only because that knowledge makes it easier to attend to the body, but not just the diabetic body writ large—the specific body. In my interview transcripts, this physically situated knowledge was often expressed with the phrase “for me.” (p. 90). The diabetic body may be a complex assemblage, but a diabetic body is always a specific assemblage, having continuities and discontinuities with other bodies.
Data Resonance
Diabetes is at once extremely personal as a disease that must be self-managed (with diabetics describing themselves, for instance, as their “own experiments” (Arduser, 2017, p.96)), and it is also inevitably shared with others in the healthcare community, family and friends. My earlier example of other people recognizing my lows demonstrates this, and serves as another instance of the excorporation of the metabolic body described by Mol and Law (2004, p. 52). Thus, the very personal body is not formed in opposition to the world outside it, not in conflict with its surroundings, not a resolutely self-contained individual. Writing on a wide array of prostheses, from limb replacements to drugs, Shildrick (2015) argues that such things “not only demonstrate the inherent plasticity of the body, but, in the very process of incorporating non-self matter, point to the multiple possibilities of co-corporeality, where bodies are not just contiguous and mutually reliant but entwined with one another. Against a modernist convention of fully bounded bodies, separate and distinct from one another, such modes of corporeal transformation comprehensively undo the limits of the embodied self” (p. 16). Shildrick’s assertion is particularly forceful when also paired with Law and Mol’s (2004) discussion of the body’s excorporation of actions, where “some bodily activities may take place beyond the surface of the skin” (p. 52). Diabetes suggests that the idea of the personal body and the idea of co-corporeality are not mutually exclusive.
Hemo-resonance #1 plays on this dynamic by working with one individual’s personal data set – my own – and simultaneously following and generating connections to other bodies, both human and non-human. In using my personal data, the work links into the wider cultural logic of self-tracking, invested in n=1 bodily experimentation. In this context, data visualizations are becoming more and more pervasive as ways of displaying and interpreting large amounts of data. As an alternative to the pervasiveness of visualization, I have decided to delve into data resonance. The affective connotations of “resonance”, the notions of amplification and attenuation, extension in time, and movement (both physical and emotional), make it apt as a way of shifting attention from the laser-focus on fidelity, precision, transparency, and legibility to a larger field of affects that arise from, and give rise to, data. Sharing something with Lupton’s “data sense” in its engagement with embodied, affective and material aspects of data, data resonance also differs in that it is less concerned with interpretation, sense-making and knowledge. Data resonance focuses on movements and performances of and with data. It does not operate in opposition to data visualization, but instead re-orients it. Dominant diabetic data visualizations have provided important insights for diabetes self-management. Jeff Kanter, of Databetes, has created some of the most inventive and appealing visualizations of diabetic data. Adhering to the Quantified Self mantra – “Self-knowledge through numbers” – such visualizations are primarily intended to provide people with new ways of understanding their bodily data in order to make better decisions in the future. A visualization that makes data less legible is generally not regarded as effective in this context. Unconcerned with legibility, data resonance produces visualizations and other manifestations of data that aim to detach themselves as much as possible from goal-orientation, following instead other possible trajectories of data and bodies. This is akin to Gouge and Jones’ (2018) discussion of wearables and the difference between “screened wearing”, which considers data within a representationalist framework, and “diffractive wearing”, which focuses on relationships and on how data is part of larger systems of activity with import beyond representing and controlling bodies (p. 422). Like diffractive wearing, data resonance can be posed as “a kind of productive interference…which in failing to do what was intended, at the same time makes visible relationships that are obscured or minimized” (p. 431). In other words, data resonance as it operates in Hemo-resonance #1 “misuses” diabetic data in order to make room for experiencing and reflecting on other relationships that the self-management of diabetes might reveal.
For Hemo-resonance #1, visualization is achieved by first sonifying the data – assigning pitches and durations to the blood glucose readings and insulin injection amounts – and then making those sonifications tactile. Inspired by the work of David Bobier of Vibrafusionlab, I played the data-as-sound back through tactile transducers, devices designed specifically to transfer audio signals to physical vibrations in materials other than air. Such transducers cause objects to vibrate based on sound signals. In Hemo-Resonance #1, the sound signals generated by the sonification of diabetic data are transferred as physical vibrations to a cardboard surface on which the hundreds of test strips used to perform blood-glucose measurements are laid out. Normally discarded as biomedical waste, the test strips are now animated, given another life, by the very data they helped to produce. Their reactions to the vibrations are video-recorded and subsequently processed to produce a mirrored effect, creating the impression of a pattern where in reality the motion of the strips was chaotic. This series of transferences from data to sound to physical vibration to object movement to visual display is instructive of data resonance – data moves from one place and mode of existing to another creating specific, yet not fully predictable effects as it does so.
The other major data resonance of the work lies in the tactile transducers that users are invited to touch to their bodies. Here, visitors feel the vibrations of the data – data that charts the expansion of the body beyond the skin barrier via blood-glucose readings and insulin injections – at the same time as they see the effects on the test strips in the video. Because human bodies and test strips are composed of vastly different materials, the way the vibrations move through them varies tremendously. The result is that sometimes what visitors feel seems synchronized to what they see and sometimes it does not, producing shifting dis/congruences. Data resonance happens at multiple places at once, creating linked but variable effects. The peering into the body effected through blood sugar tests and the recording of insulin injections is presented as circulatory, constantly in motion, provoking variable responses in different bodies, human and non-human.
Although the work seems to start with the numerical data and channel it through various pathways to achieve its effects, Hemo-resonance #1 is as much a meditation on how these numbers are generated. The body performs the numbers in collaboration with other people and things in the world – the capacities of the strips and meter, the testing protocols, the archiving and recording protocols, all of which are continually on the move. Diabetic data is co-created and the technologies that “collect” it are as Mol (2009) puts it, “erratic” and “never quite tamed” (p. 1757); ways of generating and communicating the data are always changing. For my part, I generated very different data in the days when I manually recorded my blood sugar readings, insulin injections, and carbohydrate consumption in a physical log book than I do now with my data management largely delegated to, and delimited in various ways by my glucose meter. Data resonance is both about the effects of data in the world and how it is affected and comes into being. To play on Paterson’s (2007) discussion of the resonance of flesh, drawing on Maurice Merleau-Ponty, we could say that just as flesh has resonance, data “has a resonance, a vibration, a texture of its own that responds to the textures of the world” (p. 161-162).
Arduser (2017) has characterized diabetes as a state of permanent liminality (p.14), and she quotes a TuDiabetes forum participant who refers to it as “predictably unpredictable” (p. 28). Diabetes is ongoing, and although control may be the prized goal, it can never be achieved once and for all. What works today may not work tomorrow. The liminality of diabetes is also more than perpetual adjustments to self-management. The process of doing diabetes involves the constant travels of data as they come into the world and produce effects in the world, and as they move between thresholds drawing bodies together. It involves fluids trespassing the skin barrier, and the diabetic extending (or excorporating) her body to touch others around her, whether she wants to or not. The liminality is the weave of shifting and boundary-challenging relations that doing diabetes produces. In Hemo-resonance #1, I have attempted to follow some of these relations through the resonance of data. In diabetes management, the diabetic’s particular bodily configurations, perceptions, knowledge, and data are continually put in the service of achieving an end result – target blood sugar levels matching as closely as possible those of a “normal” body. Hemo-resonance #1 attempts to provide a space for attending to diabetes apart from this goal-orientation, to remain more resolutely in the multiple liminalities of diabetes.
Non-concluding Patterns
Diabetes management involves the constant search for patterns, as the diabetic attempts to correlate different sources of data to attain tighter control of her condition. Though the patterns are in perpetual flux, as diabetics we are nevertheless trained to continuously look for them, to attend to an interlacing of numbers and feelings to better understand and act on our disease. The routine search for patterns becomes as embodied as the finger-pricks and insulin injections – part of our performance of diabetes, a kind of style of perceiving the world. Hemo-resonance #1 makes patterns uninterpretable, emptying them of instructive content, while maintaining the structure of a pattern and the changeability of the body. It attempts to take up the ongoing-ness of diabetes without determining where it is heading. In the face of pressures to better ourselves through interpretations of numbers, the work offers a space for something else to take place. On the one hand, it is a response to the cultural thrust towards surveilling bodies through numbers for improved health and fitness, and the ableist attitudes expressed therein. On the other hand, it is not a reaction in that it does not argue back – it does not take a normative stand. It is not saying what we should or should not do. Instead, it plays with the modes of perception and bodily conditions of diabetes in an attempt to make room for what might emerge from these ways of being in the world besides healthist orientations. It echoes in some ways Sanders’ (2017) call for self-trackers to take up their data in more experimental ways that take the body as “eternally (trans-)forming” but not as something to perfect (p. 56-57). And it resonates with Gouge and Jones’ (2018) emphasis on embodied interactions with devices and environments that involve “inventional disruption of categories and metrics” (p. 427). The work opens a space for becoming, not in the sense of becoming better, but in the sense of continuous liminality, unpredictability, and relationality. Such spaces are required not just as psychological salves or therapeutic meditations for the diabetic who has become distressed in their never-ending search for control, but more broadly, as spaces where we continue to ask about the boundaries and configurations of humans and non-humans, and where we recognize the value of bodily difference.
Endnote
- Documentation of Hemo-resonance #1 can be accessed at: https://samuelthulin.com/projects/hemo-resonance-1/. My second work in the series (not discussed in this article) Hemo-resonance #2 can be accessed at: https://samuelthulin.com/projects/hemo-resonance2/
References
- Arduser, L. (2017). Living Chronic: Agency and Expertise in the Rhetoric of Diabetes (1 edition). Columbus: Ohio State University Press.
- Bennett, J. A. (2019). Managing Diabetes: The Cultural Politics of Disease. NYU Press.
- Bruni, A., & Rizzi, C. (2013). Patient 2.0 and the Re-engineering of Clinical Encounters. Science & Technology Studies, 26(1), 29–43.
- Elman, J. P. (2018). “Find Your Fit”: Wearable technology and the cultural politics of disability. New Media & Society, 20(10), 3760–3777. https://doi.org/10.1177/1461444818760312
- Forlano, L. (2017). Data Rituals in Intimate Infrastructures: Crip Time and the Disabled Cyborg Body as an Epistemic Site of Feminist Science. Catalyst: Feminism, Theory, Technoscience, 3(2), 1–28. https://doi.org/10.28968/cftt.v3i2.28843
- Garland -Thomson, R. G. (1997). Extraordinary Bodies: Figuring Physical Disability in American Culture and Literature. New York: Columbia University Press.
- Gouge, C., & Jones, J. (2018). Wearable Technologies and Invention. Rhetoric Review, 37(4), 421–433. https://doi.org/10.1080/07350198.2018.1497887
- Horrocks, S. (2019). Materializing datafied body doubles: Insulin pumps, blood glucose testing, and the production of usable bodies. Catalyst: Feminism, Theory, Technoscience, 5(1), 1–26.
- Kafer, A. (2013). Feminist, Queer, Crip. Indiana University Press.
- Kowalski, A. J. (2019). Realizing Better Diabetes Outcomes Through a Diabetes Data Revolution. Diabetes Spectrum, 32(3), 179–181. https://doi.org/10.2337/ds19-0004
- Kuppers, P. (2007). The Scar of Visibility: Medical Performances and Contemporary Art (First edition edition). Minneapolis: Univ Of Minnesota Press.
- Lupton, D. (2012). Medicine as culture: Illness, disease, and the body (3rd ed). Los Angeles: SAGE.
- Lupton, D. (2013). Quantifying the body: Monitoring and measuring health in the age of mHealth technologies. Critical Public Health, 23(4), 393–403. https://doi.org/10.1080/09581596.2013.794931
- Lupton, D. (2014a). Apps as Artefacts: Towards a Critical Perspective on Mobile Health and Medical Apps. Societies, 4(4), 606–622. https://doi.org/10.3390/soc4040606
- Lupton, D. (2014b). Beyond Techno-Utopia: Critical Approaches to Digital Health Technologies. Societies, 4(4), 706–711. https://doi.org/10.3390/soc4040706
- Lupton, D. (2017). Feeling your data: Touch and making sense of personal digital data. New Media & Society, 19(10), 1599–1614. https://doi.org/10.1177/1461444817717515
- Maturo, A., Moretti, V., & Mori, L. (2016). An Ambiguous Health Education: The Quantified Self and the Medicalization of the Mental Sphere. Italian Journal of Sociology of Education, 8(3), 248–268. https://doi.org/10.14658/pupj-ijse-2016-3-12
- Mol, A. (2009). Living with diabetes: care beyond choice and control. The Lancet, 737, 2.
- Mol, A., & Law, J. (2004). Embodied Action, Enacted Bodies: The Example of Hypoglycaemia. Body & Society, 10(2–3), 43–62. https://doi.org/10.1177/1357034X04042932
- Moretti, V., & Morsello, B. (2017). Self–management and Type 1 Diabetes: How Technology Redefines Illness. TECNOSCIENZA Italian Journal of Science and Technology Studies, 8(1), 51–71.
- Paterson, M. (2007). The Senses of Touch: Haptics, Affects and Technologies (1 edition). Oxford ; New York: Bloomsbury Academic.
- Piras, E. M., & Miele, F. (2017). Clinical self-tracking and monitoring technologies: Negotiations in the ICT-mediated patient–provider relationship. Health Sociology Review, 26(1), 38–53. https://doi.org/10.1080/14461242.2016.1212316
- Samuels, E. (2003). MY BODY, MY CLOSET: Invisible Disability and the Limits of Coming-Out Discourse. GLQ: A Journal of Lesbian and Gay Studies, 9(1–2), 233–255. https://doi.org/10.1215/10642684-9-1-2-233
- Sanders, R. (2017). Self-tracking in the Digital Era: Biopower, Patriarchy, and the New Biometric Body Projects. Body & Society, 23(1), 36–63. https://doi.org/10.1177/1357034X16660366
- Scheiner, G. (2011). Think like a pancreas: A practical guide to managing diabetes with insulin (1st Da Capo Press ed., completely rev. and updated). Boston, MA: Da Capo Lifelong.
- Shildrick, M. (2015). “Why Should Our Bodies End at the Skin?”: Embodiment, Boundaries, and Somatechnics. Hypatia, 30(1), 13–29. https://doi.org/10.1111/hypa.12114
- Smith, G. J. D. (2016). Surveillance, Data and Embodiment: On the Work of Being Watched. Body & Society, 22(2), 108–139. https://doi.org/10.1177/1357034X15623622
- Smith, G. J. D., & Vonthethoff, B. (2017). Health by numbers? Exploring the practice and experience of datafied health. Health Sociology Review, 26(1), 6–21. https://doi.org/10.1080/14461242.2016.1196600
- van der Ploeg, I. (2012). The body as data in the age of information. In K. Ball, K. Haggerty, & D. Lyon (Eds.), Routledge Handbook of Surveillance Studies (1st ed., pp. 176–183). https://doi.org/10.4324/9780203814949
- Wendell, S. (2001). Unhealthy Disabled: Treating Chronic Illnesses as Disabilities. Hypatia, 16(4), 17.